Discitis, or disc space infection, is an inflammatory condition that affects the intervertebral disc space located between two vertebrae, or bones, of the spine. Characterized by the slow onset of severe back pain, discitis is most often seen in children under 10; however, adults may develop the condition, as well.
What Is Discitis?
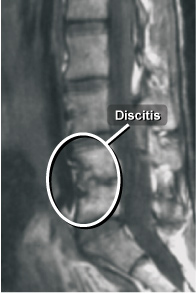
Discitis, or disc space infection, is an inflammatory condition that affects the intervertebral disc space located between two vertebrae, or bones, of the spine. Discitis may be caused by a bacterial or viral infection, or other inflammatory processes such as those associated with autoimmune disease. The condition most commonly affects the discs in the lumbar (low back) and thoracic (middle/upper) portions of the spine.
Discitis can be very painful; the pain also tends to be aggravated by movement of the spine and often radiates to other parts of the body such as the abdomen, hip, leg or groin.
What Are The Symptoms Of Discitis?
In addition to back pain, symptoms of discitis may include:
- Fever
- Chills
- Sweating
- Stiffness
- Fatigue
- Loss of appetite
Young children with this condition may act irritable and uncomfortable and refuse to sit up, stand or walk.
How Is Discitis Diagnosed?
To determine if discitis is the cause of you or your child’s back pain or other symptoms, your doctor may prescribe one or more of the following tests:
- X-ray – to check for narrowing of the disc space between vertebrae
- MRI (Magnetic Resonance Imaging) – to check for inflammation of the disc space
- Bone Scan – which may reveal increased uptake at the inflammation site
- CBC (Complete Blood Count) – to check for an elevated white blood cell count
- ESR (Erythrocyte Sedimentation Rate) – to check for an elevated sedimentation rate, an indicator of inflammation
How Is Discitis Treated?
The goal of treating discitis is to eliminate the cause of the inflammation and reduce the pain and other symptoms. Antibiotics, anti-inflammatory and pain relief medication and/or steroids may be prescribed. Bed rest and the use of a brace for immobilization and support of the affected area also may be recommended.
A full recovery can be expected in cases that involve infection. In instances in which discitis has developed as a result of an autoimmune disease, recovery may depend on management of that disease, as most autoimmune conditions are typically chronic.
Discuss your condition thoroughly with your doctor, and rely on his or her judgment regarding which treatment option is most appropriate.
